Instructions for Use
Definitions of Symbols on Device Label
 | Catalog Number |
 | Batch Code / Lot Number |
 | Serial Number |
 | Use by Date |
 | Sterilized Using Irradiation |
 | Do Not Reuse |
 | Consult Instructions for Use |
 | Manufacturer |
 | MR Conditional (see page 8) |
 | Do Not Use if Package is Damaged |
 | Do Not Re-Sterilize |
 | Authorized Representative in the European Community |
Description
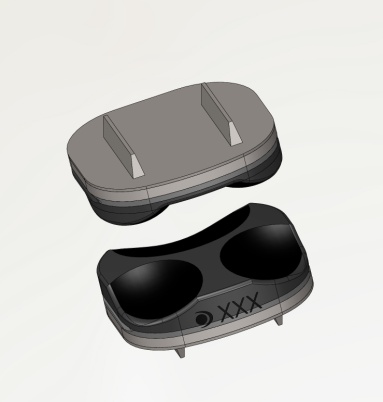
The DymicronTM Triadyme cTDR is a two-piece articulating artificial disc prosthesis. The device is implanted in place of the natural intervertebral disc using an anterior cervical approach. Initial fixation is provided by dual keels, anchored in each of the superior and inferior vertebral body endplates. Long term fixation is achieved through osseo integration of CP (Commercially Pure) Titanium plasma spray into bone ingrowth surfaces.
The articulation mechanism of the device consists of three spherical lobes mating to three non-congruent, spherical pockets. The natural motion of the cervical spine motion segment is approximated by the motion of the three lobes within their associated pockets.
Each half of the Triadyme cTDR is a sintered monobloc, consisting of a polycrystalline diamond (PCD) bearing surface with a base of titanium-titanium carbide composite. The Ti-TiC base (including the mounting keels) is CP titanium plasma spray coated. Four different footprint sizes are available for the device, with two different disc heights for each footprint, accommodating a wide variety of vertebral sizes.
The cTDR is a self-centering device. The full ranges of motion are indicated:
| Flexion/Extension | Lateral Bending | Rotation | Translation |
|---|---|---|---|
| ±6º | ±6º | ±12º | ±1mm |
ID Height
(mm)Footprint Size
(Width x Length)Catalog Number
6NS 6 14.5mm x 13mm CS-6A
6NL 6 14.5mm x 15mm CS-6B
6WS 6 16.5mm x 13mm CS-6C
6WL 6 16.5mm x 15.5mm CS-6D
7NS 7 14.5mm x 13mm CS-7A
7NL 7 14.5mm x 15mm CS-7B
7WS 7 16.5mm x 13mm CS-7C
7WL 7 16.5mm x 15.5mm CS-7D
Customized instrumentation is needed to properly install the Triadyme cTDR, minimally including a Trial, Chisel, and Inserter. Each instrument is designed for implanting a particular size of device, and should not be used to implant other sizes.
Indications for Use
The Triadyme Cervical Total Disc Replacement is indicated in skeletally mature patients for reconstruction of the disc from C3-C7 following discectomy for intractable Symptomatic Cervical Disc Disease (SCDD). Symptomatic cervical disc disease is defined as neck or arm (radicular) pain and/or a functional/neurological deficit with at least one of the following conditions confirmed by radiographic (CT, MRI, x-ray, etc.) studies: herniated nucleus pulposus, spondylosis (indicated by the presence of osteophytes), or loss of disc height. The Triadyme Cervical Total Disc Replacement is implanted via an open anterior approach. Patients receiving the Triadyme Cervical Total Disc Replacement should have failed at least six weeks of non-operative treatment for Symptomatic Cervical Disc Disease prior to implantation.
Contraindications
The Triadyme Cervical Disc Replacement should not be implanted in patients with the following conditions:
•Active systemic infection or infection localized to the site of implantation
•Allergy or sensitivity to the implant materials (titanium or cobalt)
•Osteoporosis, defined as a DXA bone mineral density T-score equal to or less than -2.5
•Marked cervical instability on radiographs (e.g., radiographic signs of subluxation greater than 3.5 mm or angulation of the disc space more than 11 degrees greater than adjacent segments)
•Severe spondylosis characterized by bridging osteophytes or an absence of motion (less than 2 degrees)
•Significant cervical anatomical deformity or compromised vertebral bodies at the index level (e.g., ankylosing spondylitis, rheumatoid arthritis, or compromise due to current or past trauma)
•Significant kyphotic deformity or significant reversal of lordosis
Precautions
Patient selection is extremely important. In selecting patients for a total disc replacement, the following factors can be of extreme importance to the success of the procedure: the patient’s occupation, activity level, and general health, as well as the presence of senility, mental illness, alcoholism, or drug abuse. In addition, certain degenerative diseases (e.g., degenerative scoliosis or ankylosing spondylitis) may be so advanced at the time of implantation that the expected useful life of the device is substantially decreased. Medical conditions such as Alzheimer’s disease and emphysema may affect postoperative management.
In order to minimize the risk of periprosthetic vertebral fractures, surgeons must consider all co-morbidities, past and present medications, previous treatments, etc. Surgeons should screen patients to determine if a DXA bone mineral density measurement is necessary. If DXA is performed, the patient should not receive the Triadyme Cervical Disc (as noted in the contraindications above) if the DXA bone mineral density T-score is equal to or less than -2.5. It may be advisable, at the surgeon’s discretion, to exclude patients with a T-score less than -1.0.
The safety and effectiveness of this device has not been established in patients with the following conditions:
•Skeletal immaturity (less than 21 years of age) or advanced age (60 years or older)
•Axial neck pain as solitary symptom
•Neck or arm pain of unknown etiology
•More than one cervical level with DDD
•Facet joint disease or degeneration of involved vertebral bodies
•Prior surgery at the level to be treated
•Prior spinal fusion at an adjacent cervical level
•Clinically significant cervical instability
•Taking medication known to potentially interfere with bone or soft tissue healing (e.g., steroids)
•Less than six weeks of non-surgical treatment
•Extreme obesity, as defined by the NIH Clinical Guidelines Body Mass Index (a BMI of 40 or greater)
•Rheumatoid arthritis or other autoimmune disease
•Active malignancy
•Paget’s disease, osteomalacia, or other metabolic bone disease
•Chronic or acute renal failure or history of renal disease
•Unstable cardiac disease
•Severe, insulin-dependent diabetes
•Systemic disease, including AIDS, HIV or Hepatitis
•Pregnancy
Use aseptic technique when removing the Triadyme Cervical Disc from the innermost packaging. Also use care when handling the device to ensure that it does not come in contact with objects that could damage it. Damaged implants are no longer functionally reliable.
Take care to ensure that blood or other debris are not trapped between the bearing surfaces of the assembled device.
It has been reported in the literature that short-term postoperative use of non-steroidal anti-inflammatory drugs (NSAIDs) may reduce the instance of heterotopic ossification.
Implanted metal alloys release metallic ions into the body. The long term effects of these ions on the body are not known.
Surgical implants must never be re-used or re-implanted. Although the device may appear undamaged, it could have small defects and/or internal stress patterns that may lead to early breakage.
The components of Triadyme Cervical Disc should not be used with components or instruments of spinal systems from other manufacturers. See the surgical manual for step-by-step instructions.
Patients should be instructed in postoperative care procedures and should be advised of the importance of adhering to these procedures for successful treatment with the device. Patients should be advised against any activities that require repeated bending, lifting, and twisting, such as athletic activities. Gradual increases in physical activity will depend on individual patient progress and monitoring the device for stability and proper functioning.
Potential Adverse Events
Potential risks associated with the use of the Triadyme cTDR device include: 1) those commonly associated with any surgery; 2) those specifically associated with cervical spinal surgery using an anterior approach; and 3) those associated with a spinal implant, as well as those pertaining to the Triadyme cTDR. However, the causality of these adverse events is not exclusive to these categories.
There is also the risk that this surgical procedure will not be effective, and may not relieve or may cause worsening of preoperative symptoms.
- Risks associated with any surgical procedure including: abscess; cellulitis; wound dehiscence; wound necrosis; edema; hematoma; heart and vascular complications; cerebrovascular complications including ischemia, stroke, hemorrhage, and thrombosis; hypertension; embolism; thromboembolism; thrombophlebitis; adverse reactions to anesthesia; gastrointestinal complications; pulmonary complications; organ, nerve, or muscular damage; seizure, convulsion, or changes to mental status; and complications of pregnancy including miscarriage and fetal birth defects.
- Risks associated with anterior interbody surgery of the cervical spine include: dysphagia; dysphasia; dysphonia; hoarseness; vocal cord paralysis; laryngeal palsy; sore throat; recurring aspirations; nerve deficits or damage; tracheal, esophageal, and pharyngeal perforation; airway obstruction; external chylorrhea; warmth or tingling in the extremities; deficit or damage to the spinal cord, nerve roots, or nerves possibly resulting in paralysis or pain; dural tears or leaking;
cerebrospinal fistula; discitis, arachnoiditis, and/or other types of inflammation; loss of disc height; loss of proper curvature, correction, height or reduction of the spine; vertebral slipping; scarring, herniation, or degeneration of adjacent discs; surrounding soft tissue damage, spinal stenosis; spondylolysis; otitis media; fistula; vascular damage and/or rupture; and headache. - Risks associated with implants in the spine, including the Triadyme cTDR device, are: early or late loosening of the components; disassembly; bending or breakage of any or all of the components; implant migration; malpositioning of implant;
loss of purchase; sizing issues with components; anatomical or technical difficulties; implant fracture; bone fracture; skin penetration, irritation, pain, bursitis resulting from pressure on the skin from component parts in patients with inadequate tissue coverage over the implant; foreign body reaction to the implants including possible tumor formation, autoimmune disease, metallosis, and/or scarring; possible tissue reaction; bone resorption; bone formation that may reduce spinal motion or result in a fusion, either at the treated level or at adjacent levels; development of new radiculopathy; myelopathy or pain; cessation of bone growth of the operated portion of the spine; tissue or nerve damage caused by improper positioning and placement of implants or instruments; loss of neurological function; decreased strength of extremities; decreased reflexes; appearance of cord or nerve root injury; loss of bladder control or other types of urological system compromise; gastrointestinal system compromise including loss of bowel control; reproductive system compromise including erectile dysfunction, altered sensation, and loss of ability to achieve orgasm. - Loss and/or interference with radiographic and other imaging modalities because of the presence of the implant.
- Wound, local, and/or systemic infections.
- Surgical instrument bending or breakage, as well as the possibility of a fragment of a broken instrument remaining in the patient.
- Inability to resume activities of normal daily living, including loss of consortium.
- Death
How Supplied
•The DymicronTM Triadyme Cervical Disc is supplied sterile and is single use only. Do not re-sterilize or reuse the Triadyme Disc. Re-sterilizing and/or reusing the DymicronTM Triadyme Cervical Disc may result in impaired performance and could cause patient injury and/or the communication of infectious diseases between patients.
•Do not use the DymicronTM Triadyme Cervical Disc after the last day of the month of the “Use by date” on the label.
•Inspect the device package before opening. Do not use if package is damaged or shows any evidence of breached packaging, compromised device sterility.
•Use sterile technique to carefully remove the disc from the packaging. Inspect the Triadyme Cervical Disc to ensure it exhibits no signs of damage.
•Once removed from the package, keep the Triadyme Cervical Disc from coming into contact with any cloth, sponges, or other foreign material that may become attached to the Titanium Plasma Spray Coating of the backside.
•The DymicronTM Triadyme Cervical Disc serial number and size must be documented for each patient record.
A Patient with this device can be scanned safely, immediately after placement under the following conditions:
•Static Magnetic field of 1.5-Tesla and 3-Tesla, only
•Maximum Spatial gradient magnetic field of 18,000-Gauss/cm (extrapolated) or less
•Maximum MR system reported, whole body averaged specific absorption rate (SAR) of 2-W/kg for 15 minutes of scanning (i.e., per pulse sequence
•Normal Operating Mode of Operation for the MR system
-
WARNING:
Correct installation and placement of the device is essential to optimal performance. Implanting the Triadyme Cervical Disc should only be attempted by surgeons who are thoroughly knowledgeable about spinal anatomy and biomechanics, have experience with anterior cervical spinal surgeries, and have hands-on training in the use of this specific device. A lack of adequate experience and/or training may lead to higher incidences of adverse effects, including neurological complications.
Correct selection of the appropriate implant size is extremely important to assure the proper placement and function of the device. See the surgical technique manual for step-by-step instructions for selecting and implanting an appropriately sized Triadyme Cervical Disc.
Due to the proximity of vascular and neurological structures to the implantation site, there are risks of serious or fatal hemorrhage as well as risks of neurological damage with the use of this device. Care must be taken to identify and protect these structures during surgery. Serious or fatal hemorrhage may occur if the great vessels are eroded or punctured during implantation and subsequently damaged due to breakage of implants, migration of implants, or if pulsatile erosion of the vessels occurs because of close apposition of the implants.
All surgical waste materials (including device packaging) must be considered bio-hazardous and disposed of according to applicable national or regional regulations.
The Triadyme Cervical Disc is a single use device; under no circumstances should the device be transplanted or reused in any way. It is not possible to reliably clean and/or sterilize a Triadyme Cervical Disc after it has been previously implanted in a patient, and life-threatening complications can occur if reuse is attempted.
-
CAUTION:
Excessive removal of subchondral bone during the preparation of the vertebral endplates may lead to less than optimal clinical outcomes and is not recommended.
Once removed from the package, keep the Dymicron Triadyme Cervical Disc from coming into contact with any cloth, sponges, or other foreign material that may become attached to the Titanium Plasma Spray Coating of the backside. The package capsule may be used to safely store the loaded Dymicron Triadyme Cervical Disc.
The Dymicron Triadyme Cervical Disc cannot be re-positioned in an anterior direction without complete removal. Take care not to place the Dymicron Triadyme Cervical Disc too posterior.
Take care not to over-distract the disc space.
Device Retrieval
•Should it be necessary to remove a Triadyme Cervical Disc, please contact DymicronTM to receive instructions regarding the data collection, including histopathological, mechanical and adverse event information. Please refer to the Triadyme Cervical Disc Surgical Technique for device removal. All explanted devices must be returned to DymicronTM for analysis.
•Please note that the Triadyme Disc must be retrieved as carefully as possible in order to keep the Implant and surrounding tissue intact. Also please provide descriptive information about the gross appearance of the device in situ, as well as descriptions of the removal methods, e.g. intact or in pieces.
Limited Warranty
DymicronTM warrants that reasonable care has been used in the manufacture of this device. There are not express or implied warranties, including fitness for a particular purpose, for this DymicronTM Triadyme Cervical Disc system. Any description or specifications provided are solely to describe the product at the time of manufacture and do not constitute any express or implied warranties. DymicronTM is not responsible for any direct, incidental, special, or consequential loss, damage or expense based on any defect, failure or malfunction of this product, other than as expressly provided by mandatory provisions of applicable law. No person has the authority to bind DymicronTM to any representation or warranty except as provided in this Limited Warranty.
![]() Manufactured by:
Manufactured by:
DymicronTM
1186 S. 1680 W.
Orem, UT 84058, USA
Telephone: +1-801-221-4591
Fax: +1-801-426-4846
www.Dymicron.com
pdc@Dymicron.com
![]()
European Authorized Representative:
MT Promedt Consulting GmbH
Altenhofstrasse 80
66386 St. Ingbert Germany
Telephone: +49 6894 581020
www.mt-procons.com
info@mt-procons.com
©2014 DymicronTM All rights reserved. Covered by U.S. Patent No. 8,163,023 B2 and other pending U.S. and foreign patent applications. DymicronTM and Triadyme cTDR are trademarks or registered trademarks of DymicronTM.
Label #305681 Rev. E

